Scientists from University of Southampton pinpoint a cluster of biomarkers present in individuals with tuberculosis
Tuberculosis (TB) is a preventable and usually curable disease. Yet in 2022, TB was the world’s second leading cause of death from a single infectious agent, after corona virus (COVID-19). More than 10 million people continue to fall ill with TB every year. Urgent action is required to end the global TB epidemic by 2030, a goal that has been adopted by all Member States of the United Nations (UN) and the World Health Organization (WHO).

TB is caused by the bacillus Mycobacterium tuberculosis, which is spread when people who are sick with TB expel bacteria into the air (e.g. by coughing). About a quarter of the global population is estimated to have been infected with TB. Following infection, the risk of developing TB disease is highest in the first 2 years (approximately 5%), after which it is much lower. Some people will clear the infection.
Backed by the UK Medical Research Council and the NIHR, researchers worked in partnership with international specialists, among them, experts from the University of Cape Town in South Africa and Cayetano Heredia University in Peru.
It is well known that the gold standard for the diagnosis of active TB patients is sputum smear culture, which often requires 2 to 8 weeks. By employing an innovative method, the research team managed to discover a set of six proteins with high precision for detecting TB, following an analysis of proteins present in the blood of individuals with active TB from Africa and South America. It is anticipated that the testing period for detecting active TB could be shortened to merely 2 days.
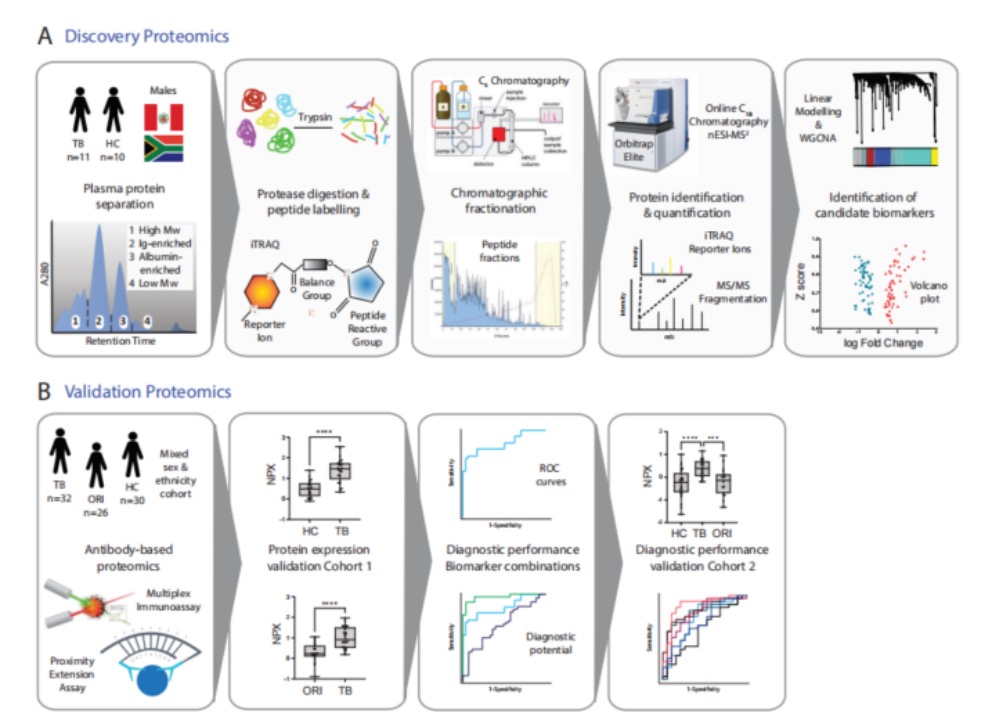
After studying proteins found in the blood of patients with active tuberculosis (TB) in Africa and South America, researchers used a new technique to identify a set of six proteins that are very accurate in identifying TB. The researchers employed a non-depleting, non-targeted proteomics approach to provide unique, high protein group coverage that can identify new markers with high sensitivity and specificity for TB. The most detailed plasma proteome for TB to date has been reported, and by using complementary antibody capture techniques, upregulated proteins were validated in a clinical cohort that includes patients with other respiratory infections, with hopes of developing it into a near-patient screening test.
After comparing biomarkers between healthy individuals and patients with lung infections, researchers identified a total of 118 proteins that showed significant differences between the groups. The researchers then narrowed these proteins down to six, which could distinguish patients with infectious tuberculosis from those in good health or with other lung diseases.
Dr. Diana Garay-Baquero, study co-director from the University of Southampton, remarked: “The novel markers we’ve identified are genuinely thrilling. The crucial next step is to transform these findings into tests accessible for the millions unknowingly carrying and spreading TB.”